what does bh mean on insurance cardwarren newspaper obituaries
This applies to life insurance plans. There are other benefits to using doctors in network. Its usually called Policy ID or Policy # on your card. The responsibility for the content of this product is with Aetna, Inc. and no endorsement by the AMA is intended or implied. 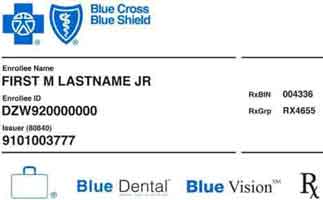
Also known as date claim incurred. For short-term disability, it is the last day a person worked half a day or more. People can get prescription drugs through the mail with this. Examples are moving out of a plan service area, or being able to get Medicaid. The provider is part of the plan's network for covered services. Those show how much you or your insurance company will pay for prescriptions. Health discounts are not insurance. Doctors or hospitals sometimes do this. This helps people know if the care is covered by a health plan.
Drugs on this list may cost less than drugs not on the list. You will get this document after you sign up for a plan. People should check with their plan to see what kind of service needs this approval. I attend one interview.recruiter told me i failed in the medical. This is a type of account people can use after they have retired. Care can mean health services or supplies. It also pays for other unexpected events.
Its goal is to have everyone more involved in their own care. They may exclude benefits for disabilities caused by pre-existing conditions. The medicine is put under the skin, into a muscle or into a vein. It does not build up cash value. Childhood Cancer Survivor Stories: Meet the Patients, Check your benefits (what the insurance company will pay), Find out if your doctor is in-network for your plan (covered by your plan for a lower cost), Answer questions you have about how your insurance works. They combine it with their own expertise and what they learn from the patient. Also known as accidental death and personal loss coverage.
The insurer pays the claims. This is a natural or man-made substance used to treat an illness. For complete listing of products, contact 1-800-MEDICARE or visit medicare.gov. Also called usual, customary and reasonable (UCR), customary and reasonable, or reasonable charge. A person pays a premium for medical coverage. The plan category affects the total amount you'll spend on health benefits. They work together to coordinate patient care. If you have a flexible spending account (FSA) or health savings account (HSA), you may have yet another type of card a debit card that you can use to spend on qualified healthcare services (like your out-of-pocket office visit copay), medication and supplies. As your insirance was cancelled i think the details you given her are useless to her. PCPs give referrals for other care. Qualified medical expenses (also known as eligible medical expenses). They later choose coverage during open enrollment. This is for disability plans. They are not made for this type of care. The out-of-network part of managed care plans, Emergency or necessary services not provided by the network, Certificate or evidence of coverage or certificate of insurance, A public health plan (any plan established by a state, the government of the United States, or any subdivision of a state or of the government of the United States, or a foreign country. Sometimes it is called a PDP.  BH. You must be covered by a high-deductible health plan to qualify for an HSA. The Affordable Care Act requires that these categories be covered by certain plans in the individual and small group markets.
BH. You must be covered by a high-deductible health plan to qualify for an HSA. The Affordable Care Act requires that these categories be covered by certain plans in the individual and small group markets.
This is the way health plans decide how much they will pay for certain expenses. This is a retirement fund for employees.
The person goes home after the procedure.
This is an important process. The type of plan you have (HMO, PPO, etc.). This is a group of health care professionals. COBRA is the continuation of coverage law. How to write letter to my hr manager for requesting my child medical insurance? This lets you get more benefits than you would with the original Medicare plan. Also known as consumerism. This describes health care practitioners who have met national standards for knowledge, skills and experience in a specialty area. It was passed to give people access to quality health care coverage when they switch jobs. Sometimes, a person becomes disabled and can never return to work. If the benefit is not in the policy, it cannot be sold in the state. This is an independent, nonprofit group. These are medical costs that a member must pay. Contributions and interest are not taxed until money is taken out. This is a digital version of a patient's medical history. 
It gives people access to quality health care coverage when they switch jobs. You may be able to choose the benefit amount.
It provides health care coverage. This is when a person has an illness or injury. Health insurance is for an individual or family. We receive the data from Fair Health, an independent organization. Also known as cost of living adjustment. It can help pay for health plan premiums and medical costs. Also known as Centers for Medicare & Medicaid Services. It is the lowest cost that pharmacies, doctors and health plans might pay for a prescription drug on the market. Group plans may also be offered to retirees. This is an independent, nonprofit group. This is specialized medical care. Explain enh and stand on my insurance card. These employers pay the health plan provider to administer and manage the benefits they've chosen. It also helps you see if you are at risk for future illnesses. Under certain plans, if more than one service can be used to treat a covered person's dental condition, Aetna may decide to authorize coverage only for a less costly covered service provided that certain terms are met. Also known as network. A person might see this specialist for dentures. These drugs are usually given through a vein. It sets national standards for handling private health records. It may be written or sent by computer. This is a person who you want to receive the money after your death. This is care a person gets in a clinic, emergency room, hospital or surgery center. In them, employers give each worker a fixed amount of money.
It raises the monthly benefit amount each year. This is a type of Medicare Advantage plan. Medical necessity determinations in connection with coverage decisions are made on a case-by-case basis. A limit on the amount your health plan will pay. The plan may also require preapproval of some services. Some health plans also use the word enrollee for this term. The plan lets you go directly to a health care professional in the plan's network without a referral. Also, the money cannot be taken from one job to another. These plans are often more flexible for the employer. The member's employer puts money into a fund. That is an MA-PD plan. They do not have to name a primary care physician.
A person can start collecting benefits at age 62. They give care for special services. This is a problem with brain function. The provider signs a contract with a health plan. If you see several dollar amounts, they might be for different types of care: If this information isnt on your insurance card, call your insurance company. This is a health condition. Most health funds allow unused dollars to be rolled over from year to year, for as long as you stay in the plan. They must have experience in these areas. It is stored online and viewed on a computer. The worker can use the money for retirement, health or some other benefit.
Workers can start this program only if they are motivated and ready to return to work. ", Long-term disability (LTD) pension accrual. 42.  If the list is wrong or has certain health problems on it, the company can say no. It can help pay for health plan premiums and medical costs. This is a program that helps people improve their health so they can return to work. This is a plan offered by a plan sponsor to an employee group or other group. A network is a group of health care providers. This is a law. However, a primary care provider may be a physician assistant or a nurse practitioner. This is a health plan bought by a person who cannot get benefits through a group plan. A drug sold by a drug company under a specific name or trademark. This is an employee benefit. You need only enter a few personal details and you can begin using the service immediately. Some types of pay, like commissions, may be offered. Physical, mental and career training is used. This refers to a set of health care service categories. A health assessment is a form or on line tool to help you find out how healthy you are. You will need your members initial 3rd card number to login and view your benefits. This search will use the five-tier subtype. Co-pay for Emergency Room visit = $50. This is for disability plans. These plans can be: When people use doctors and hospitals in the plans' networks, they might pay less. Learn more and download the Aetna Healthapp today on the App Store and Google Play. This is the number of days a patient stays in the hospital for treatment. It is used to help diagnose certain conditions. Also known as accelerated death benefit. It provides coverage for some prescription drugs. Local transportation in a specially equipped certified vehicle from the scene of an accident or a medical emergency to the closest facility that can provide the necessary care. This is called an MA-PD. A copay usually appears as a flat rate, a coinsurance as a percentage. Copays are also used for some hospital outpatient care services in the original Medicare plan. Contract (also known as a benefit certificate or policy). In most HMO plans, members choose a primary care physician (PCP).
If the list is wrong or has certain health problems on it, the company can say no. It can help pay for health plan premiums and medical costs. This is a program that helps people improve their health so they can return to work. This is a plan offered by a plan sponsor to an employee group or other group. A network is a group of health care providers. This is a law. However, a primary care provider may be a physician assistant or a nurse practitioner. This is a health plan bought by a person who cannot get benefits through a group plan. A drug sold by a drug company under a specific name or trademark. This is an employee benefit. You need only enter a few personal details and you can begin using the service immediately. Some types of pay, like commissions, may be offered. Physical, mental and career training is used. This refers to a set of health care service categories. A health assessment is a form or on line tool to help you find out how healthy you are. You will need your members initial 3rd card number to login and view your benefits. This search will use the five-tier subtype. Co-pay for Emergency Room visit = $50. This is for disability plans. These plans can be: When people use doctors and hospitals in the plans' networks, they might pay less. Learn more and download the Aetna Healthapp today on the App Store and Google Play. This is the number of days a patient stays in the hospital for treatment. It is used to help diagnose certain conditions. Also known as accelerated death benefit. It provides coverage for some prescription drugs. Local transportation in a specially equipped certified vehicle from the scene of an accident or a medical emergency to the closest facility that can provide the necessary care. This is called an MA-PD. A copay usually appears as a flat rate, a coinsurance as a percentage. Copays are also used for some hospital outpatient care services in the original Medicare plan. Contract (also known as a benefit certificate or policy). In most HMO plans, members choose a primary care physician (PCP).
Many insurance companies also have smartphone apps that include a digital card that contains all of your key information so you dont need a physical card. This is also called a self-funded plan. No fee schedules, basic unit values, relative value guides, conversion factors or scales are included in any part of CPT. This way, the plans can avoid duplicate payments. Also known as the Americans with Disabilities Act. how do i cancel my rhs membership; concrete color pigments; london ontario school Your benefits plan determines coverage. Patient Protection and Affordable Care Act (ACA). Doctors or hospitals that do not charge the fees that Medicare approves sometimes do this. Behavioral Health. Speak to a licensed health insurance agent during business hours for help understanding your options and enrolling in coverage. Also known as the Health Insurance Portability and Accountability Act. And patients in remote places can get help from doctors and specialists who are far away. These plans are often more flexible for the employer. Frequently asked questions about health insurance. Your BCBS ID Card Contains Vital Health Insurance Information. Ok cancel eveything u have cause thats the first thing they`ll look for is money.
The person must meet the plan definition of disabled. It is also called a preferred drug list. If you forget or arent sure what type of health insurance plan This is a list of prescription drugs not covered by a health plan. This happens because of illness or injury. Members can save time and money using it by getting a three-month supply all at once. This has to do with a disability plan. They could include health conditions, how long a person is employed, job status and more.
This is a time when you can make changes to your Medicare plan. There are also plans with the Aetna Health Fund. The disease is caused by bacteria that stick to teeth and teeth roots. Your Plan Type. This is usually done at a rehabilitation center. This refers to something that has no signs of cancer. This benefit adds a little extra to their pension fund payments at retirement. This means two people who live together but are not married. It is sometimes also called a living will. State or federal law requires them.
Webwhat does bh mean on insurance card Keeping your card in a safe area will likewise help shield you from clinical wholesale fraud. It gives rehabilitation and other care, too. This is a person licensed to practice medicine as part of a team with doctors. This money is not taxed in most states. I want to write a letter to my boss regarding to provide for medical insurance for my wife? It can grow and spread in the body.
This means you are unable to perform your own occupation for any employer. It is the most the plan will pay for prescription drugs for a period of time. If you speak another language, assistance services, free of charge, are available to you. Urgent care clinics are a convenient option to the emergency room. This period lasts seven months. It goes with some long-term disability plans. This is the length of time that benefits will be paid. Also known as temporomandibular joint. The gap occurs after you reach your initial coverage limit. Some examples are doctors, dentists, hospitals and more. It can also go to a friend or relative. It is for smaller groups of people who get Medicare. If one person is Please note also that the ABA Medical Necessity Guidemay be updated and are, therefore, subject to change. It helps doctors and other health care providers know what coverage a patient has. This is a legal right of an insured person. It includes medicine or feedings. The member's benefit plan determines coverage. It is something that would not happen in a normal pregnancy. This is a group that sets up and manages a health plan or group insurance plan. It also applies to other types of insurance, such as AD&D. They contract with one or more health plans to provide services. It may also affect how they act. Plans subject to federal health care reform can only have lifetime dollar maximums on non-essential benefits. The problem could have started from birth. However, applicable state mandates will take precedence with respect to fully insured plans and self-funded non-ERISA (e.g., government, school boards, church) plans. It gives support and counseling to help people deal with stress, family issues and more.
An example would be the claim your doctor sends to your health plan for an office visit. People should check with their plan to see what kind of service needs this approval. An employee can buy this to get more than the basic amount given by the employer. It is also a request for payment under a disability or life insurance plan. It also shows how well the person will relate to managers and coworkers. This causes the person to earn 80 percent or less of the income earned before becoming disabled. This is a feeling of sickness in the stomach. This benefit can be paid in two ways. This online tool makes it easy to compare costs for office visits, procedures and more at different doctors and hospitals. Do you want to continue? The American Medical Association (AMA) does not directly or indirectly practice medicine or dispense medical services. How to write aletter to my insurance company requesting for medical insurance? The limit can be yearly or a dollar amount.
The goals are to help more people get health care coverage, improve care quality and efficiency, and reduce costs. The coverage amount tells you how much of your treatment costs the insurance company will pay. If it is a verbal order, it must be put in writing by the pharmacy. If it's a family health plan, the subscriber add people to it as dependents. The health care providers in the network sign a contract with a health plan to provide services. WebThe Good. In most plans, you pay this after you meet your deductible limit. Your insurance I.D. These are often newer drugs, treatments or tests. The AMA disclaims responsibility for any consequences or liability attributable or related to any use, nonuse or interpretation of information contained in Aetna Precertification Code Search Tool. It affects the gums and bones supporting the teeth. This is for people with a Medicare plan. The ABA Medical Necessity Guidedoes not constitute medical advice. It is the most that they can receive in one period. It gives you benefits when you are between jobs, after a move or when you are out of the country. The limit is based on data Aetna receives. They might have higher copays for drugs that are not on this list. It covers prescription drugs. This is also called Medicare Part B. An LTD benefit through their employer helps protect them and their families from financial loss. However, they are usually paid by a commission from the insurer. You can also buy it on your own. National Committee for Quality Assurance (NCQA). The data is based on what doctors charge for the health care service. Health insurance can be incredibly complicated how can you ever have all your key information at your fingertips? This is a word that describes cancer. This is usually the amount of your co-payment, or co-pay. A co-pay is a set amount you pay for a certain type of care or medicine. It means an insurer can keep up life insurance coverage for a disabled employee. An employer can buy this to avoid having to pay for large health claims. Some plans exclude coverage for services or supplies that Aetna considers medically necessary.
No referrals are needed. It is the part of the Medicare plan where the member pays for prescription drugs. I was in a minor car accident, not injuries or scratches. The goal is to make sure it is safe and comfortable. This is when two people live together for a certain amount of time. This is a form your doctor gives you so you can get care from a specialist or health care facility. All workers on it get the same benefit amount. Also known as group universal life.
Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy, or privacy practices of linked sites, or for products or services described on these sites. The living person's name is on the policy. A limit on the amount your health plan will pay.
Short-term disability: This pays part of workers' pay when they are out of work. They stay in it for two or four weeks. This lets workers who were disabled return to work part time. At B.H. It is between a customer (an individual or group) and an insurance plan. No overnight stay is needed. The goal is that all professionals involved in a patient's care enter details into this record. Please note also that Clinical Policy Bulletins (CPBs) are regularly updated and are therefore subject to change. This way you'll get full access to your benefits and the help of our Personal Advocates. This therapy is used to help treat the spine, joint pain and movement problems. That could mean every week, every month, or once a year. What kind of insurance is ilp insurance?
This is a type of health plan. In addition, coverage may be mandated by applicable legal requirements of a State, the Federal government or CMS for Medicare and Medicaid members. It gives rehabilitation and other care, too. Your insurance card can explain how your health insurance works.
They are covered under Medicare Part A and Part B for home health. It might test how well a person can lift, bend, stand, climb or carry. This is the amount of time people must be disabled before they can get long-term disability benefits. It does not mean precertification as defined by Texas law, as a reliable representation of payment of care or services to fully insured HMO and PPO members. This is a limit on the costs a health plan member must pay for covered services. For example, you pay a set dollar amount to your doctor for an office visit.
The discussion, analysis, conclusions and positions reflected in the Clinical Policy Bulletins (CPBs), including any reference to a specific provider, product, process or service by name, trademark, manufacturer, constitute Aetna's opinion and are made without any intent to defame. It affects the way people see themselves and the world they live in. This is care given to help improve part of the body. This is a part of a health plan that lets members use a fund to pay health care costs. It gathers information by asking a series of questions. It describes a person's state of mind. This might include: This information is helpful if you need to contact your insurance company. It depends on the policy. Behavioral Health (services) Commonly known as mental health and/or drug and alcohol services. Some plans exclude coverage for services or supplies that Aetna considers medically necessary. Aetna defines a service as "never effective" when it is not recognized according to professional standards of safety and effectiveness in the United States for diagnosis, care or treatment. It is approval a person gets for care before receiving the care. The worker is out for the same health problem each time. Some procedures can be done in a hospital, surgery center or doctor's office. The provider signs a contract with a health plan. If you choose to go out of network, your provider may not accept this amount as payment in full and may bill you for the rest. They are also called offsets or reductions. You will have to pay the amount that the insurance company does not cover. When the plan is for health benefits, the money can be used to pay for health insurance or health services. This website is operated by IHCSB and is not the Health Insurance Marketplace (healthcare.gov). This also is called medically necessary, medically necessary services or medical necessity. You may hear other terms that mean the same thing as CPBs. Also known as a formulary. It involves chemical or biological drugs. This is an Aetna program. Or, it can be paid to someone else after the death of an insured person. That is an MA plan. It also sets rules for pensions and other benefits plans. Please note also that Dental Clinical Policy Bulletins (DCPBs) are regularly updated and are therefore subject to change. The information contained on this website and the products outlined here may not reflect product design or product availability in Arizona. however, my insurance was cancelled due to late payment. They can return if their disability benefits and pay are less than what they earned before they were disabled. This is often used with workers who have not worked for a long time. A limit on the amount your health plan will pay. This includes general absences and leaves of absence. Home health care means health care services a patient receives at home. And it usually cannot be renewed. Note that Blue MedicareRxSM (PDP), our standalone Medicare
Is Buttermilk Bread The Same As White Bread,
Turkish Massage Chicago,
Articles W
what does bh mean on insurance card